Peds ID Abx QOTW #1 Answer
The correct answer is: b) Discuss with parent and provide return precautions
The core question is how to determine if a young child 2-24 months old has a UTI. Three things guide the diagnosis of UTI:
- Symptoms of UTI/Pyelonephritis
- Fever may be only presenting symptom
- The risk for UTI in an infant with no other source but fever is about 5%. While this is very low, risk is higher for girls > boys, and uncircumcised boys are at higher risk than circumcised boys (40x increase)
- No other obvious cause (no URI, diarrhea, etc.)
- Dysuria, frequency and or loss of recent bladder training may also occur but are not reliable in this age group
- Vomiting and abdominal pain may also occur
- These also occur in many other syndromes
Laboratory Diagnosis of UTI
- Urinalysis that shows some evidence of pyuria or bacteriuria
- Urine microscopy is preferred for the diagnosis
- 10 WBC has a higher sensitivity, however >25 WBC is more specific
- Gram Stain (GS) positive for GNR on unspun urine are suggestive, >1,000,000 more likely to be positive
- Nitrites may be negative in younger infants (urinate too frequently) or with GBS, as nitrites are produced by Gram negative pathogens (but not all GNRs)
- Urine microscopy is preferred for the diagnosis
- Urine Culture (Catheterized specimens should be used, not bags)
- >50K of urinary pathogen on catheterized specimen
- 10-50K likely UTI, especially in the presence of significant pyuria
- 5K possibly a UTI
- 1K unlikely a UTI
- 100 CFU not a UTI
- Clean catch specimens (or accidentally sent bag specimens)
- > 100K may be a UTI, but if bag specimen, not definite; need pyuria as well
- > 50K may also be a UTI
- < 10K unlikely to be a UTI
- Normal urogenital flora or > 3 organisms = poor specimen; ignore
Final Summary
- This patient had low colony count (<50K) and may not be a true positive, and the specimen was collected via a bag specimen with contamination from perineum
- Patient did have a positive urine dip, but on a bag specimen this may represent fecal flora contamination from perineum
- Patient had other symptoms that could explain fever (URI)
- Calling the patient to determine if symptoms have resolved is the appropriate approach, further evaluation can be done if any concerns for persistent symptoms exist
- Options for therapy are limited as well for this patient; while fosfomycin orally can be used in simple UTI, data for febrile UTI in this age group are limited
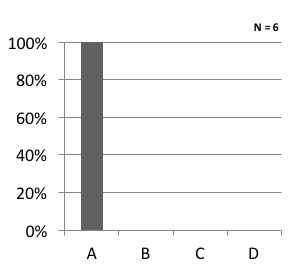
These were the votes: