Peds ID Abx QOTW #10 Answer
b) Obtain wound cultures from I&D or aspiration
e) Send home with Rx for Bactrim or Clindamycin
 How others answered
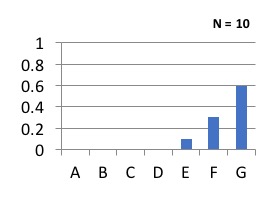
How others answered
Staphylococcus aureus Abscess
- The vast majority of patients who present with complaints of a “spider bite” have pyogenic abscess, and by far the most common cause is S. aureus, followed by Group A Streptococcus
- Community-acquired methicillin-resistant S. aureus (CA-MRSA) was by far the most common organism in the early 2000’s, peaking around 2009
- Most recent data nation wide has suggested about 40% of S. aureus is now MRSA and the remaining portion is methicillin-sensitive (MSSA)
- This is consistent with our institutional findings (see Antibiogram)
- Remember in injection drug users Gram negatives and anaerobes may also be involved in such abscesses
Management of Abscesses
- I&D has been a mainstay for large abscess without cellulitis or systemic symptoms
- Cure rates range from about 70-80% with I&D alone
- I&D or aspiration will lead to earlier symptomatic improvement
- Recent data suggests that a course of antibiotics may improve outcomes further(1,2)
- 1. Talan DA. et al. N Engl J Med 2016;374:823-32
- 2. Daum RS. et al. N Engl J Med. 2017 Jun 29;376(26):2545-2555
- While these studies used 10 days of antibiotics, we routinely use 5-7 days for skin infections, so I would recommend giving a short course of 5-7 days for abscess that requires I&D
- Further data is needed to determine the appropriate length of therapy post I&D
- For small abscess (<2cm) with or without cellulitis a short course of 5-7 days of antibiotics is likely to be effective
- Abscess with systemic symptoms should be given IV antibiotics with I&D until bacteremia is ruled out
Case Discussion
- Blood cultures & admission are not necessary without systemic symptoms
- However, this patient is young with a large abscess (would consider this moderate disease); it would be prudent to get a culture to guide future therapy options
- IV therapy is unnecessary if you have an option that is likely to work against MRSA in this context
- At our institution, TMP-SMX has >95% activity against MSSA and MRSA
- Clindamycin overall is effective against all S. aureus but we do not have data to separate outpatient & inpatient isolates
- Equal effectiveness was seen for Clindamycin and TMP-SMX regardless of the organism, suggesting that TMP-SMX is effective for Group A streptococcus
- Cephalexin is unnecessary to be added to TMP-SMX based on DMID study(1)
- 1. Miller LG. et al. N Engl J Med. 2015 Mar19;372(12):1093-103
- Cephalexin alone does not have adequate coverage for MRSA, which still represents 40% of S. aureus abscess